Immersion Behavior Study of Hydroxyapatite Scaffolds Derived from Bovine Sources In Acidic, Basic, and Neutral Solutions
DOI:
https://doi.org/10.59535/faase.v2i1.296Keywords:
Calcination, Hydroxyapatite, Immersion, PorosityAbstract
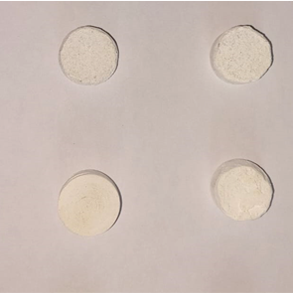
This research investigates the effects of particle size and compaction pressure on the dissolution behavior of hydroxyapatite scaffolds synthesized from bovine bone in acidic neutral and basic solutions. Hydroxyapatite was extracted through a process involving cutting, cleaning, boiling, soaking in NaOH, sun drying, grinding into powder and calcination at 800°C. The powder was then sieved into two size fractions (75 and 150 microns) and compacted at pressures of 200, 250, and 300 MPa. The mass and dimensions of the scaffolds were measured to calculate porosity, followed by immersion in the respective solutions for 24 hours to determine dissolution rates. Results indicated that smaller particle sizes and higher compaction pressures resulted in reduced porosity and enhanced structural integrity. The dissolution rates varied significantly with pH levels, exhibiting the highest rates in acidic conditions up to 215.83 mg/cm2 and the lowest in basic solutions up to 11.32 mg/cm2. Additionally, scaffolds with smaller particles and higher compaction pressures demonstrated lower dissolution rates across all pH levels due to lower porosity. In conclusion, both particle size and compaction pressure are critical factors influencing the dissolution behavior of hydroxyapatite scaffolds. These findings have significant implications for the design and optimization of hydroxyapatite-based materials for biomedical applications, where controlled dissolution rates are crucial for performance and longevity.
Downloads
References
A. Szcześ, L. Hołysz, and E. Chibowski, “Synthesis of hydroxyapatite for biomedical applications,” Advances in Colloid and Interface Science, vol. 249. Elsevier B.V., pp. 321–330, Nov. 01, 2017. doi: 10.1016/j.cis.2017.04.007.
G. Chandra and A. Pandey, “Biodegradable bone implants in orthopedic applications: a review,” Biocybernetics and Biomedical Engineering, vol. 40, no. 2. Elsevier Sp. z o.o., pp. 596–610, Apr. 01, 2020. doi: 10.1016/j.bbe.2020.02.003.
M. Prakasam, J. Locs, K. Salma-Ancane, D. Loca, A. Largeteau, and L. Berzina-Cimdina, “Fabrication, Properties and Applications of Dense Hydroxyapatite: A Review,” J Funct Biomater, vol. 6, no. 4, pp. 1099–1140, Dec. 2015, doi: 10.3390/jfb6041099.
H. Shi, Z. Zhou, W. Li, Y. Fan, Z. Li, and J. Wei, “Hydroxyapatite based materials for bone tissue engineering: A brief and comprehensive introduction,” Crystals, vol. 11, no. 2. MDPI AG, pp. 1–18, Jan. 01, 2021. doi: 10.3390/cryst11020149.
B. Beig, U. Liaqat, M. F. K. Niazi, I. Douna, M. Zahoor, and M. B. K. Niazi, “Current challenges and innovative developments in hydroxyapatite-based coatings on metallic materials for bone implantation: A review,” Coatings, vol. 10, no. 12. MDPI AG, pp. 1–29, 2020. doi: 10.3390/coatings10121249.
V. S. Kattimani, S. Kondaka, and K. P. Lingamaneni, “Hydroxyapatite–-Past, Present, and Future in Bone Regeneration,” Bone Tissue Regen Insights, vol. 7, p. BTRI.S36138, Jan. 2016, doi: 10.4137/btri.s36138.
J. Lamsihar Manalu, B. Soegijono, and D. J. Indrani, “Characterization of Hydroxyapatite Derived from Bovine Bone,” 2015. [Online]. Available: www.ajouronline.com
E. Fiume, G. Magnaterra, A. Rahdar, E. Verné, and F. Baino, “Hydroxyapatite for biomedical applications: A short overview,” Ceramics, vol. 4, no. 4. MDPI, pp. 542–563, Dec. 01, 2021. doi: 10.3390/ceramics4040039.
A. Mocanu et al., “Ion release from hydroxyapatite and substituted hydroxyapatites in different immersion liquids: In vitro experiments and theoretical modelling study,” R Soc Open Sci, vol. 8, no. 1, Jan. 2021, doi: 10.1098/rsos.201785.
M. Figueiredo, S. Cunha, G. Martins, J. Freitas, F. Judas, and H. Figueiredo, “Influence of hydrochloric acid concentration on the demineralization of cortical bone,” Chemical Engineering Research and Design, vol. 89, no. 1, pp. 116–124, Jan. 2011, doi: 10.1016/j.cherd.2010.04.013.
D. O. Obada, E. T. Dauda, J. K. Abifarin, D. Dodoo-Arhin, and N. D. Bansod, “Mechanical properties of natural hydroxyapatite using low cold compaction pressure: Effect of sintering temperature,” Mater Chem Phys, vol. 239, Jan. 2020, doi: 10.1016/j.matchemphys.2019.122099.
W. Khoo, F. M. Nor, H. Ardhyananta, and D. Kurniawan, “Preparation of Natural Hydroxyapatite from Bovine Femur Bones Using Calcination at Various Temperatures,” Procedia Manuf, vol. 2, pp. 196–201, 2015, doi: 10.1016/j.promfg.2015.07.034.
S. Mondal, U. Pal, and A. Dey, “Natural origin hydroxyapatite scaffold as potential bone tissue engineering substitute,” Ceram Int, vol. 42, no. 16, pp. 18338–18346, Dec. 2016, doi: 10.1016/j.ceramint.2016.08.165.
J. Fan et al., “In Vivo Biocompatibility and Improved Compression Strength of Reinforced Keratin/Hydroxyapatite Scaffold,” Tissue Eng Regen Med, vol. 15, no. 2, pp. 145–154, Apr. 2018, doi: 10.1007/s13770-017-0083-9.
H. Lee, T. S. Jang, J. Song, H. E. Kim, and H. Do Jung, “The production of porous hydroxyapatite scaffolds with graded porosity by sequential freeze-casting,” Materials, vol. 10, no. 4, Mar. 2017, doi: 10.3390/ma10040367.
A. Sobczak-Kupiec, E. Olender, D. Malina, and B. Tyliszczak, “Effect of calcination parameters on behavior of bone hydroxyapatite in artificial saliva and its biosafety,” Mater Chem Phys, vol. 206, pp. 158–165, Feb. 2018, doi: 10.1016/j.matchemphys.2017.12.020.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Komang Widhi Widantha

This work is licensed under a Creative Commons Attribution 4.0 International License.
By submitting a manuscript to Frontier Advances in Applied Science and Engineering (FAASE), the author(s) agree to the following terms:
-
Copyright: The author(s) retain copyright to their work, granting Frontier Advances in Applied Science and Engineering (FAASE) the right to publish it. Articles are licensed under a Creative Commons Attribution 4.0 International License (CC BY).
-
License Grant: The CC BY license allows others to share and adapt the work for any purpose, even commercially, provided proper attribution is given to the original author(s) and the source, a link to the Creative Commons license is provided, and any changes made are indicated.
-
Author's Rights: Authors are allowed to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work, with proper acknowledgment of its initial publication in Frontier Advances in Applied Science and Engineering (FAASE).
-
Permissions: Reproduction, posting, transmission, or other distribution or use of the final published article, in whole or in part, requires prior written permission from Frontier Advances in Applied Science and Engineering (FAASE) and the respective author(s).
-
Attribution: Proper attribution must be given to the original author(s) and the source, indicating that the work was originally published in Frontier Advances in Applied Science and Engineering (FAASE) with a link to the published article.
-
No Warranty: The journal and its editorial team make no representations or warranties regarding the accuracy, completeness, or fitness for a particular purpose of the published work.
-
Dispute Resolution: Any disputes arising from the use of the licensed material shall be governed by the laws of [Jurisdiction] without regard to conflicts of law principles.
By submitting a manuscript to FAASE, the author(s) agree to abide by these license terms and grant the necessary rights to Frontier Advances in Applied Science and Engineering (FAASE) for the publication and dissemination of the submitted work.










